How Beneficial is Fish Oil?
by Neil Docherty

Fish oil is the third most widely used supplement in the United States, with around 10 percent of Americans taking it regularly — often for the perceived benefit to cardiovascular health.
But there are two big problems when it comes to fish oil: Researchers still cannot definitely say whether it actually lowers the risk of heart attack and stroke. And even if they could, there can be big differences between the fish oil that is prescribed to patients by their physicians, and some versions of the supplement that are available over-the-counter.
Preston Mason of the Harvard Medical School explains the distinction in the above scene from the new FRONTLINE documentary, Supplements and Safety, which premieres tonight on most PBS stations (check local listings).
It comes down to oxygen, says Mason. Fish oil is extracted as a byproduct from oily fish like anchovies. As the fish are crushed, they’re exposed to air, meaning the oil becomes oxidized. That can turn the smell of fish oil rancid, which is one thing, but more worrisome is that oxidized fish oil contains oxidized lipids, which can trigger changes inside human cells that lead to health problems like cardiovascular disease.
Prescription-grade fish oil needs to be approved by the Food and Drug Administration, notes Mason, and because the approval process comes with stringent production standards, the risk of oxidation runs low. However, in Mason’s work and in other previously published studies, researchers have found that the type of fish oil that’s sold in stores often has high levels of oxidation.
Even if oxidation weren’t an issue, some say there is still no conclusive evidence that the supplement can ward off a heart attack. Among those experts is the University of Aukland’s Andrew Grey, who in a 2014 study in JAMA Internal Medicine reviewed seven years worth of fish oil research published in top medical journals. Grey found that in all but two studies, researchers could not show that fish oil was any more effective in preventing cardiovascular events in high-risk populations than a placebo.
“I think for cardiovascular disease, one has to say, there is no compelling evidence that taking fish oil protects against the first heart attack or a second heart attack,” Grey told FRONTLINE in an interview for Supplements and Safety. “And so, people who are advised to do that, or are doing it, are wasting their time. And their money.”
Adam Ismail, executive director of the GOED fish oil trade association questions that conclusion, telling FRONTLINE, “There’s certainly ample evidence that it helps things like reducing blood pressure, reducing your risk of coronary health.” It’s hard to argue, Ismail added, that the omega-3s found in fish oil “aren’t important for how your heart functions.”
Still, until a clearer link can be established, researchers like Grey and Mason say that eating fish may just be the better option.
Vitamin D, fish oil supplements don't benefit cardiovascular health, new study finds
For decades, doctors have been searching for a surefire way to prevent atrial fibrillation, an abnormal heart rhythm that can prove fatal. Now, a new, high-quality study has ruled out two possible contenders: vitamin D and fish oil supplements.

The trial, called VITAL-Rhythm, took center stage at a recent virtual conference of the American Heart Association (AHA), the nation's largest professional organization of doctors who focus on the heart and cardiovascular system.
"Atrial Fibrillation is a very common condition and is hard to treat," said Dr. Christine Albert, the study's lead author and chair of the Department of Cardiology in the Smidt Heart Institute at Cedars-Sinai. "There are an estimated 33 million people in the world with atrial fibrillation."
Atrial Fibrillation is not benign, she explained. If left untreated, it can lead to serious health consequences such as stroke, heart attacks, heart failure, dementia, and even death. Although early, less reliable studies hinted that vitamin D and fish oil might help, doctors said this new study shows they don't make a difference.
Doctors said it's a relief to see high-quality evidence like this, because it means they can focus on new research frontiers, and avoid prescribing unnecessary pills to their patients.
Prior studies identified a possible link between these supplements and atrial fibrillation rates, but it wasn't clear if these differences were caused by the supplements themselves, or by some other unexplained factor, such as lifestyle choices.
Albert and her research team embarked on a massive study comprised of 25,000 volunteers, who would be randomly selected to receive vitamin D, fish oil or a placebo pill.
Dr. Erin Michos, the director of women's cardiovascular health and the associate director of preventive cardiology at the Ciccarone Center for the Prevention of Cardiovascular Disease at Johns Hopkins University Medical Center, said the study received praise at this year's American Heart Association conference because it was a high-quality study that included diverse volunteers. This means that the findings are applicable regardless of race and gender.
"They studied vitamin D at 2000 IU per day compared to placebo, while simultaneously studying 840 milligrams a day of marine Omega-3s vs placebo. This was a randomized clinical trial and blinded, so participants did not know whether they were taking a supplement or placebo," Michos said.
Historically, large trials have been victim to underrepresentation and lack of diversity, making it difficult for clinicians to apply these trials to their true patient population. This study, meanwhile, represented a larger population of African Americans and women.
An undated stock photo of fish oil supplements. STOCK/Getty Images
Michos said that the importance of having a strong representation of African Americans in this trial was critical. Many have a lower blood levels of vitamin D as a result of darker skin pigmentation, which leads to poor absorption of UVB light, which is necessary to create active vitamin D and utilize its benefits.
"I actually applaud the study investigators for their efforts in diversity in this trial," Michos said. "Twenty percent enrollment of Blacks means they were overrepresented relative to their proportion in the U.S. population."
In addition, Michos said that women are frequently underrepresented in cardiovascular trials, which usually limits doctors' understanding of whether a drug or treatment will work just as well in women as it does in men.
"However, this was not the case in VITAL- Rhythm trial," Michos said. "The VITAL trial enrolled 51% women."
In recent years, research has shown a behavioral shift among some Americans toward a rise in the consumption of supplements: an estimated 120 billion dollar industry.
But researchers say the true health benefits of supplements are often overstated.
"For the vast majority of supplements, there does not appear to be any benefit. Again, more is not better if one does not have a nutritional deficiency. Some high dose supplements can even cause harm," Michos said.
The evidence is growing that supplements do not prevent primary or repeated cardiovascular disease. Another study debut at AHA, the OMEMI trial, showed no benefit in adding marine n-3 polyunsaturated fatty acids supplements to prevent a second heart attack.
But what has been shown, repeatedly, is the benefit of diet and exercise in preventing, or at times even reversing, conditions like atrial fibrillation.
"We tend to look for the magic nutrient so we do not have to eat good food," Albert said.
Albert said the most effective prevention is maintaining a healthy weight, reducing alcohol intake to 1-2 drinks per day and maintaining a healthy blood pressure.
Michos agreed, she advised that a healthy lifestyle and dietary behaviors can prevent not only atrial fibrillation, but cardiac disease overall.
"Moderate exercise, following a healthy diet, maintaining a normal weight can decrease the risk of atrial fibrillation. I think the individuals would be better served by saving their money on supplements, which have not been shown to work, and instead focus their time and money on activities that promote a healthy lifestyle," she said.
Lily Nedda Dastmalchi, D.O., M.A., is an internal medicine resident physician at The George Washington University and a contributor to the ABC News Medical Unit.
Pro- and antiarrhythmic properties of a diet rich in fish oil
Abstract
Increased consumption of fish rich in omega-3 polyunsaturated fatty acids (ω3-PUFAs) is associated with decreased incidence of sudden cardiac death in post-myocardial infarction patients, but is also related to increased incidence of sudden death and arrhythmias in patients with acute myocardial ischemia. This review discusses the possible pro- and antiarrhythmic mechanisms of ω3-PUFAs in relation to various cardiac pathologies. Differences between circulating and incorporated ω3-PUFAs with respect to electrophysiology are emphasized. We conclude that ω3-PUFAs alter cardiac electrophysiology and thereby may be pro- or antiarrhythmic, dependent on the mechanism of arrhythmia. As ω3-PUFAs may be antiarrhythmic under conditions that favour triggered activity, they may facilitate re-entrant arrhythmias. This may explain the contradictory outcomes of increased intake of fish oil on sudden death and arrhythmias in clinical trials. Advice to increase intake of ω3-PUFA supplements or fatty fish should be tailored to individual patients with respect to the arrhythmogenic mechanisms associated with the underlying pathology.
1. Introduction
Epidemiological studies support the protective effect of omega-3 polyunsaturated fatty acids (ω3-PUFAs) on cardiac death and, more specifically, on sudden cardiac death [1]. The Physicians Health Study reported that eating fish at least once a week was associated with a reduced risk of sudden cardiac death, but not of myocardial infarction in men [1]. In particular men with high blood levels of ω3-PUFAs had risk reductions of sudden death up to 90% [2]. As sudden cardiac death is in the majority of cases preceded by ventricular arrhythmias, it has been suggested that ω3-PUFAs are antiarrhythmic.
The risk reductions in sudden death by ω3-PUFAs were confirmed in several randomized controlled trials [3,4]. In DART, men with a prior MI were advised to increase their fatty fish intake. 2 years later, a 29% reduction in all-cause mortality was observed in the fish advised group compared to the control group [3]. The GISSI-Prevenzione Trial, a randomized clinical trial, investigated the effects of ω3-PUFAs supplements in the secondary prevention of myocardial infarction [4]. Treatment with ω3-PUFAs lowered mortality and sudden cardiac death was reduced by 45% [4].
Following publication of these data, the American Heart Association issued an advise to eat (fatty) fish at least two times a week [5]. Patients with documented coronary heart disease are recommended by the American Heart Association to consume about 1 g of fish oil fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) per day. Fig. 1 displays the structural formulas of EPA and DHA.
Fig. 1 Open in new tabDownload slide Structural formulas of fish oil fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
Fig. 1 Open in new tabDownload slide Structural formulas of fish oil fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
Contrary to reports on the beneficial effects of fish oil, DART-2 reported that fish oil supplementation resulted in an increase in cardiac death in patients with angina pectoris [6]. Moreover, in patients with implanted cardioverter defibrillators (ICDs) fish oil supplementation resulted in a pro-arrhythmic response [7]. Two other trials reported that fish oil supplementation in patients with ICDs did not result in a pro- or antiarrhythmic response [8,9]. A systematic review concluded that additional intake of ω3-PUFAs does not have clear effects on mortality and cardiovascular events [10]. The reduction in cardiovascular mortality by ω3-PUFAs may be limited to a population subgroup (e.g. patients with myocardial infarction and with heart failure) [10]. Indeed, fish oil supplementation reduced sudden cardiac death in post myocardial infarction patients [4] while an increased risk of cardiac death was observed in patients with angina pectoris [3,6]. This may be related to different mechanisms of the prevailing arrhythmia in these population subgroups. Arrhythmias in heart failure are induced by triggered activity [11,12], while those in acute myocardial ischemia are caused by reentry [13].
Increased mortality has also been observed in several antiarrhythmic drug trials [14–17]. The main reason for the disappointing outcomes in these trials is that drugs that suppress one type of arrhythmia may facilitate another. As a consequence, the Sicilian Gambit Working Group initiated a rational approach to study antiarrhythmic drugs against the background of various arrhythmia mechanisms and their vulnerable parameters [18]. A similar approach is required to study the effects of fish oil supplementation on arrhythmias.
In this paper we review the electrophysiological effects of ω3-PUFAs in fish oil, EPA and DHA, against the vulnerable parameters of life-threatening arrhythmias. Differences between circulating and incorporated ω3-PUFAs on electrophysiology are emphasized. Modulating factors of the autonomic nervous system and intracellular pathways are outside the scope of this review.
2. Arrhythmogenic mechanisms
Arrhythmia mechanisms are traditionally divided into abnormalities in impulse initiation (triggered activity, automaticity) and abnormalities in impulse conduction (reentry) [19]. Life-threatening arrhythmias are predominantly caused by triggered activity and reentry. This review limits itself to these mechanisms. Abnormal automaticity only plays a minor role in the sub-acute phase of ischemia and does not lead to life-threatening arrhythmias [13] and thus has minor relevance on the effects of fish oil on sudden cardiac death in the population.
2.1. Triggered activity and reentry mechanisms
Triggered activity may arise from early and delayed afterdepolarizations [20]. An early afterdepolarization (EAD, Fig. 3, panel A (top)) occurs when the action potential is prolonged during slow cardiac rhythms [21]. They may give rise to a particular polymorphic ventricular tachycardia named Torsade des Pointes after its typical appearance of the electrocardiogram. The congenital or acquired long-QT syndrome is a predisposing disorder which can lead to ventricular tachycardia and ultimately sudden death from these arrhythmias. One of the antiarrhythmic interventions for EADs is action potential shortening.
Fig. 3 Open in new tabDownload slide A; Early afterdepolarization (EAD, top panel) and delayed afterdepolarization (DAD, bottom panel). B; Schematic representation of normal conduction and a reentrant circuit. C; Normal ventricular action potential (top panel). Numbers denote the different phases of the ventricular action potential. The underlying ionic membrane currents and their schematic time course (bottom panel). See text for identification of the currents.
Fig. 3 Open in new tabDownload slide A; Early afterdepolarization (EAD, top panel) and delayed afterdepolarization (DAD, bottom panel). B; Schematic representation of normal conduction and a reentrant circuit. C; Normal ventricular action potential (top panel). Numbers denote the different phases of the ventricular action potential. The underlying ionic membrane currents and their schematic time course (bottom panel). See text for identification of the currents.
A delayed afterdepolarization (DAD, Fig. 3, panel A (bottom)) can occur during rapid rhythms when intracellular Ca2+ is elevated e.g. in heart failure. Antiarrhythmic interventions for DADs include action potential shortening, slowing heart rate, lowering intracellular Ca2+ and reducing cardiac excitability. Both types of afterdepolarizations may form the trigger for a re-entrant arrhythmia.
In normal heart, an impulse is generated by the sinus node and dies out when the whole heart has been activated. Reentry occurs if the same impulse continues to re-excite tissue. It is a mechanism for the maintenance of arrhythmias (Fig. 3, panel B). Conditions that favour a re-entrant circuit to arise are slow conduction and short refractory periods (the mathematical product of conduction velocity and refractory period –the wavelength– determines the length of the circle) [13]. In addition, the presence of a unidirectional block is prerequisite for a re-entrant circuit to arise [22].
2.2. Action potential duration, excitability and conduction velocity
Interventions aimed to alter action potential duration, excitability and conduction velocity can have both pro- and antiarrhythmic actions, depending on the mechanism of arrhythmia. Action potential shortening is antiarrhythmic when the underlying arrhythmia is caused by triggered activity initiated by EADs or DADs. However, action potential shortening promotes reentry by shortening the refractory period and, therefore, the wavelength. Conversely, action potential prolongation is an antiarrhythmic strategy for reentry, but may induce EADs and thereby Torsade de Pointes.
Reducing cardiac excitability is an antiarrhythmic intervention when the underlying arrhythmia is based on triggered activity. However, it may also slow conduction, one of the conditions that favour reentry.
In the following section we review the effects of fish oil on arrhythmogenesis, vulnerable parameters of arrhythmias [18], sarcolemmal ionic currents and intracellular Ca2+ handling. We will make a distinction between acute administrations of ω3-PUFAs to ventricular myocytes and ω3-PUFAs incorporated into the sarcolemma of ventricular myocytes caused by a dietary intervention with fish oil. These treatments have dissimilar electrophysiological consequences although they are often presented as counterparts.
3. Experimental studies of fish oil on arrhythmias and electrophysiology
3.1. Fish oil and experimental arrhythmias
McLennan et al. [23] studied arrhythmias, induced by myocardial ischemia, in rats fed a 3-month diet rich in tuna fish oil, sunflower oil, or sheep fat. Only rats fed the tuna fish oil rich diet were protected from ischemia- and reperfusion-induced ventricular fibrillation [23]. Identical experiments in marmoset monkeys showed that a long term diet (30 months) rich in tuna fish oil decreased ventricular fibrillation threshold and resulted in a lower incidence of sustained ventricular fibrillation [24]. A diet rich in fish oil protected rabbits against dofetilide-induced Torsade de Pointes [25].
Not only a diet, but also intravenous administration of a fish oil emulsion reduces cardiac arrhythmias. Intravenous administration of EPA or DHA was studied in a dog model of cardiac sudden death where anterior myocardial infarction was created surgically. A hydraulic inflatable cuff was placed around the left circumflex artery so it could be compressed at will [26]. After recovery from surgery, the dogs were trained to run on a treadmill. During the final minute of a 20-minute episode of exercise, the circumflex artery was occluded. Dogs with reproducible ventricular fibrillation were selected for the experiments. Intravenous administration of EPA or DHA prevented fatal ischemia-induced arrhythmias [26]. An uncontrolled pilot study in patients with ICDs who had repeated episodes of ventricular tachycardia showed that infusion of ω3-PUFAs during electrophysiological testing reduced the inducibility of sustained ventricular tachycardia in 5 out of 7 patients [27]. However, an important drawback of these two infusion studies is that pro-arrhythmia cannot be revealed as a direct consequence of the study designs. In cellular experiments, acute administration of EPA reduced the incidence of DADs in isolated myocytes from rabbits with heart failure [28].
A meta-analysis evaluating the effects of fish oil on arrhythmia outcome in various animal studies concluded that EPA and DHA can prevent arrhythmias in ischemia- but not reperfusion-induced arrhythmia models [29]. However, this study did not discriminate between dietary administration of fish oil and direct infusion of fish oil in the different animal models.
3.2. Action potential duration, excitability and conduction velocity
Acute administration of 5–25 μM ω3-PUFAs resulted in action potential shortening in neonatal rat cardiomyocytes, rabbit ventricular myocytes and guinea pig ventricular myocytes, respectively [30–32]. Action potential shortening caused by superfusion of 10 μM EPA was accompanied by a threefold increase in relative refractory period in neonatal rat cardiomyocytes [31]. Normally, this phenomenon is referred to as post-repolarization refractoriness and is only present in depolarized cells during myocardial ischemia [13]. However, the increase in relative refractory period occurred at normal resting membrane potentials and can, therefore, only be explained by reduced membrane excitability [31].
Incorporated ω3-PUFAs, resulting from a diet rich in fish oil in pigs, also lead to action potential shortening in isolated ventricular myocytes [33]. Rabbits fed a diet rich in α-linolenic acid (ALA), an ω3-PUFA from flaxseed, had shorter QT intervals compared to the control [30].
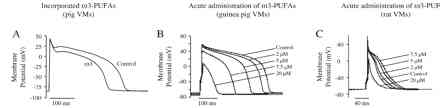
On the contrary, direct infusion of (1–20 μM) ALA and EPA prolonged QTc in isolated rabbit hearts [34]. Also, in adult rat ventricular myocytes, an increase in action potential duration was observed with low (<10 μM) ω3-PUFA concentrations, whereas action potential duration was decreased with higher (>10 μM) ω3-PUFA concentrations [32,35]. Therefore, ω3-PUFAs may shorten or prolong action potential duration, depending on differences in species and on whether they are circulating (through acute administration) or incorporated into the sarcolemma (dietary administration). Fig. 2 shows typical examples of APD changes in response to either incorporated or acutely superfused ω3-PUFAs.
Fig. 2 Open in new tabDownload slide A; Action potentials recorded from isolated ventricular myocytes from pigs fed a control diet (control) or a diet rich in fish oil (ω3). Incorporation of ω3-PUFAs results in action potential shortening. B; Action potentials recorded after acute administration of different concentrations of ω3-PUFAs in guinea pig ventricular myocytes. Acute administration of ω3-PUFAs results in action potential shortening. C; Action potentials recorded after acute administration of different concentrations of ω3-PUFAs in adult rat ventricular myocytes. Acute administration of ω3-PUFAs results in both prolongation and shortening of the action potential. Adapted from Ref. [32], with the permission of Elsevier.
Fig. 2 Open in new tabDownload slide A; Action potentials recorded from isolated ventricular myocytes from pigs fed a control diet (control) or a diet rich in fish oil (ω3). Incorporation of ω3-PUFAs results in action potential shortening. B; Action potentials recorded after acute administration of different concentrations of ω3-PUFAs in guinea pig ventricular myocytes. Acute administration of ω3-PUFAs results in action potential shortening. C; Action potentials recorded after acute administration of different concentrations of ω3-PUFAs in adult rat ventricular myocytes. Acute administration of ω3-PUFAs results in both prolongation and shortening of the action potential. Adapted from Ref. [32], with the permission of Elsevier.
Membrane excitability in single cardiomyocytes was reduced following acute administration of fish oil fatty acids EPA and DHA (5–10 μM) [31]. EPA stabilized the resting membrane potential and increased diastolic stimulation threshold [31]. This finding is in line with observations in Langendorff-perfused rabbit hearts, where direct infusion of (1–20 μM) EPA and DHA increased the threshold for induction of a ventricular extrasystole in a concentration-dependent manner [34]. Contrarily, excitability of ventricular myocytes isolated from pigs fed a diet rich in fish oil was unchanged by incorporated ω3-PUFAs [33]. In the same model, maximal upstroke velocity remained the same, suggesting that a diet rich in fish oil does not modify conduction velocity.
Direct addition of DHA (1–20 μM) to the perfusate of spontaneously beating isolated rabbit hearts resulted in a reduction of longitudinal and transversal conduction velocities, although the latter to a lesser extent [34]. This may point to reduced sodium channel availability [34] and/or reduced gap junction conductance. At present, the effect of fish oil on gap junction intracellular communication is unknown. Results of fish oil on sodium channels are reviewed in the following section.
In conclusion, fish oil alters vulnerable parameters important in arrhythmogenesis, dependent on the manner of administration. Alterations in transmembrane currents underlie these changes.
3.3. Ion channels, exchangers and intracellular calcium handling
Fig. 3, panel C illustrates the cardiac ventricular action potential (top). The numbers 0–4 define the various phases of the action potential. They respectively represent: The upstroke of the action potential (phase 0); Initial rapid repolarization, also denominated as the notch of the action potential (phase 1); The action potential plateau, or persistent depolarization of the action potential, (phase 2); Rapid repolarization (phase 3) and diastole (phase 4) [36]. The time courses of the most relevant transmembrane currents that underlie the ventricular action potential are shown in the bottom panel. Inward, depolarizing currents are schematically represented by a downward deflection. Outward, repolarizing currents are represented by an upward deflection.
3.3.1. Sodium current
The cardiac sodium current (I Na ) is responsible for the upstroke of the action potential and plays an important role in impulse conduction (Fig. 3, panel C). Peak I Na was reduced by 51% after acute administration of EPA and DHA (5–10 μM) in neonatal rat cardiomyocytes [37]. In addition, these concentrations of EPA and DHA shifted steady-state inactivation by ∼20 mV towards more negative potentials, without modifying activation properties. Similar results were obtained in human embryonic kidney (HEK293t) cells upon expression of the pore-forming subunit cDNA of the human cardiac sodium channel, hH1α, in HEK293t cells [38]. I Na was suppressed in a concentration and voltage-dependent manner by extracellular application of EPA. Furthermore, steady state inactivation of I Na was shifted by ∼27 mV towards more negative potentials. EPA enhanced slow inactivation and markedly prolonged recovery from inactivation of hH1α [38]. Several other ω3-PUFAs had similar effects on hH1α as EPA [38]. Generally, ω3-PUFAs showed higher affinity to block channels that were in the inactivated state compared to channels in closed or resting state [38]. Interestingly, substitution of a single amino acid, asparagine with lysine at site 406 (N406K) in the D1-S6 region of hH1α reduced the potency of EPA to inhibit I Na suggesting a direct interaction between EPA and the ion channel protein [39]. Activation properties of the sodium channel were unaltered by acute administration of EPA and DHA in both neonatal rat cardiomyocytes and HEK293t cells expressing hH1α cDNA, respectively [37,38]. However, in adult rat ventricular myocytes, acute administration of ω3-PUFAs (25 μM) shifted the voltage dependence of activation of the cardiac sodium channel to more positive potentials [40]. In this study, the effects of EPA and DHA on the cardiac sodium channel correlated with their ability to increase membrane fluidity [40]. Mutations in the α-subunit of human cardiac Na+ channel cause an inactivation-deficient Na+ channel with a long-lasting persistent I Na . This late I Na was more sensitive to suppression by ω3-PUFAs (IC 50 <1 μM) compared to the corresponding peak I Na (IC 50 <5 μM) in HEK-293t cells [41].
In contrast with the acute effects, peak I Na was unaffected by incorporated ω3-PUFAs in ventricular myocytes isolated from pigs and rats that were fed a diet rich in fish oil [33,42]. In both studies voltage dependence of activation remained unaltered, whereas a shift (<8 mV) in inactivation towards more negative potentials was observed [33,42].
In conclusion, acutely administered ω3-PUFAs reduce I Na [37,38,40]. This contributes to the observed reduction in excitability and to the slowing of ventricular conduction [31,34]. However, incorporated ω3-PUFAs do not alter I Na [33,42].
3.3.2. Calcium current (L- and T-type)
The L-type calcium current (I Ca,L ) is responsible for the plateau and contributes to the duration of the ventricular action potential (Fig. 3, panel C).
I Ca,L was suppressed by acute administration of ω3-PUFAs in a concentration-dependent manner (IC 50 <10 μM) in ventricular myocytes (neonatal rat, adult rat and guinea pig) [32,43,44]. Activation properties of I Ca,L remained unchanged, and a negative shift of steady-state inactivation was observed following acute administration of ω3-PUFAs [43]. Block of I Ca,L by acutely administered DHA (10 μM) was also demonstrated by Ferrier et al. [44] in guinea pig ventricular myocytes. Remarkably, ω3-PUFAs reduced I Ca,L , while preserving myocardial function [44].
Incorporation of ω3-PUFAs into the sarcolemma also reduced I Ca,L (∼20%), leaving activation properties unaltered [33]. At plateau potentials, ‘reopening’ of the L-type calcium channel was reduced in ventricular myocytes with incorporated ω3-PUFAs compared to the control VMs [33]. This may prevent EAD formation and thereby triggered activity [33].
The effects of acute and incorporated ω3-PUFAs on T-type calcium channels of the heart have not yet been described. However, it appears that the effects of acutely administered EPA and DHA on adrenal T-type calcium channels are similar to those described for L-type calcium channels [45].
In conclusion, acute administration of ω3-PUFAs to ventricular myocytes reduces I Ca,L [43,44] and thereby lowers the plateau of the action potential. Incorporated ω3-PUFAs also reduce I Ca,L and, more importantly, inhibit ‘reopening’ of the calcium channel at plateau potentials. This may prevent EADs and Torsade de Pointes [33].
3.3.3. Repolarizing currents
Early rapid repolarization or the notch of the action potential (phase 1) is caused by the transient outward current, carried by potassium ions (I to1 ) and/or chloride ions (I Cl(Ca) or I to2 ) (Fig. 3, panel C). I to is larger in subepicardial ventricular myocytes compared to mid- and endomyocardial ventricular myocytes and thereby contributes to transmural dispersion in repolarization [46]. The slow and rapid components of the delayed rectifier current (I Ks and I Kr , respectively) are responsible for rapid repolarization (phase 3) of the action potential. The inward rectifier current (I K1 ) contributes to the terminal phase of repolarization and to the maintenance of the resting membrane potential.
The Kv4.3 gene encodes a large proportion of the ion channel responsible for I to1 . DHA blocked the Kv4.3 current in a concentration dependent manner with an IC 50 of ∼4 μM in a stable transfected mammalian cell line [47]. I to1 was inhibited following acute administration of EPA and DHA (IC 50 <10 μM) in rat and ferret ventricular myocytes [32,35,48]. In the presence of the antioxidant alpha-tocopherol, the inhibiting effect of DHA on I to1 is less pronounced, but still significant in rat ventricular myocytes [49]. However, incorporated ω3-PUFAs did not alter I to1 in ventricular myocytes isolated from rats fed a diet rich in fish oil [33].
Block of I to1 would be expected to attenuate transmural dispersion of repolarization and thereby prevent reentrant tachyarrhythmias [46] but so far the effects of fish oil on transmural dispersion of repolarization have not been investigated.
I K decreased following acute administration of EPA and DHA with an IC 50 of 20 μM in ferret cardiomyocytes [48]. I K consists of two components I Kr and I Ks . Acutely administered DHA (10 μM) blocked the human ether-a-go-go-related gene (HERG) channel which encodes the pore-forming subunit of the ion channel carrying I Kr in a time-, voltage- and use-dependent manner [50]. These data suggested that DHA preferentially binds to the open state of the channel [50]. However, incorporated ω3-PUFAs did not cause any change in I Kr of pig ventricular myocytes [33].
I Ks has been studied in Xenopus oocytes upon expression of the channel pore-forming subunit, KvLQT1, in the presence or absence of the auxiliary subunit, hminK. I Ks was enhanced (∼32%) by acute administration of DHA (20 μM), but not by EPA [51]. Upon incorporation of ω3-PUFAs, I Ks was increased (∼70%) in pig ventricular myocytes [33].
A decrease of I Kr following acute administration of ω3-PUFAs may, at least in part, explain why ω3-PUFAs prolong the action potential as less repolarizing current is present during the repolarization phase of the action potential. On the other hand, augmentation of I Ks by acutely administered ω3-PUFAs leads to increased repolarizing current during the repolarization phase of the action potential. Whether the observed changes in repolarizing potassium currents caused by ω3-PUFAs lead to action potential prolongation or shortening will largely depend on the delicate balance between these and other depolarizing and repolarizing currents, species-differences regarding channel protein expression and the concentration of EPA and DHA in the superfusate [32].
I K1 did not change upon acute administration of ω3-PUFAs in ferret cardiomyocytes [48]. Incorporation of ω3-PUFAs resulted in an increase of I K1 by ∼50% in ventricular myocytes isolated from pig fed a diet rich fish oil [33]. Increased I K1 by incorporated ω3-PUFAs contributes to the observed action potential shortening [33]. In addition, an increase in I K1 may decrease excitability and thereby reduce DADs and triggered activity.
The transient outward current is not always carried by potassium ions but is, in several species, carried by chloride ions (I Cl(Ca) ) [33]. Data on I Cl(Ca) following acute administration of ω3-PUFAs are lacking. Incorporation of ω3-PUFAs into ventricular myocytes left I Cl(Ca) unaltered [33].
Other currents that affect action potential shape and duration, e.g. ultra-rapid delayed rectifier K+ current, have not yet been investigated in the presence of (circulating or incorporated) ω3-PUFAs.
3.3.4. Na+/Ca2+ exchanger
The Na+/Ca2+ exchanger (NCX) exchanges 3 Na+ ions for 1 Ca2+ ion and is therefore electrogenic. It can generate inward or outward current and contributes to the shape and duration of the action potential (Fig. 3, panel C).
Outward and inward Na+/Ca2+ exchanger current (I NCX ) was inhibited by acute administration of ω3-PUFAs (IC 50 <1 μM) in HEK293t cells [52].
Leifert et al. showed that a diet rich in fish oil increased the time constant of decay of Ca2+ transients in response to caffeine in isolated rat cardiomyocytes and suggested that NCX was involved [53]. This finding was supported by experiments in ventricular myocytes, where both outward and inward I NCX were reduced by ∼60% in the presence of incorporated ω3-PUFAs [33].
Inhibition of I NCX results in action potential shortening because less depolarizing current is available during the final repolarizing phase of the action potential (Fig. 3) [33,52]. Furthermore, I NCX contributes to DAD formation after spontaneous sarcoplasmic reticulum Ca2+-release. Possibly, reduced I NCX by both acute administration and incorporated ω3-PUFAs reduce DADs and triggered activity. Iso- and lusitropic effects of fish oil are outside the scope of this review. An antiarrhythmic action of fish oil may occur together with negative lusitropy.
3.3.5. Calcium homeostasis and sarcoplasmic reticulum function
Intracellular Ca2+ handling plays an important role in the genesis of triggered activity [54]. In experiments on rat ventricular myocytes, acute administration of EPA (1.5–15 μM) reduced the amplitude of Ca2+ transients and Ca2+ sparks without modifying Ca2+ spark kinetics [43]. The frequency of spontaneous waves of Ca2+-release was also diminished in the presence of EPA (10 μM). This indicates that sarcoplasmic reticulum function is affected by acute administration of EPA. Additionally, EPA decreased diastolic Ca2+ concentrations and imaging of Ca2+ waves showed that EPA also increased Ca2+ wave amplitudes and propagation [55]. Increased Ca2+ wave amplitudes by EPA correlated with enhanced sarcoplasmic reticulum load in rat ventricular myocytes [55–57]. It was concluded that ω3-PUFAs reduce sarcoplasmic reticulum Ca2+ uptake and also inhibit Ca2+-release (ryanodine receptors (RyR). The potency of ω3-PUFAs (10–100 μM) to reduce open probability (P o ) of RyR was demonstrated in isolated sarcoplasmic reticulum vesicles [56,58].
Spontaneous Ca2+-release from the sarcoplasmic reticulum underlies DAD-related arrhythmias in heart failure [12,59]. Increased diastolic Ca2+ levels have been shown to induce spontaneous Ca2+-releases from the sarcoplasmic reticulum in a rabbit model of heart failure [12]. In that model, diastolic and systolic [Ca2+] i levels were reduced after acute administration of EPA (20 μM) to isolated ventricular myocytes [28]. Furthermore, spontaneous Ca2+-releases and DADs were reduced by EPA after burst-pacing in the presence of noradrenalin [28].
In contrast, incorporated ω3-PUFAs did not cause any alterations in diastolic Ca2+ or Ca2+ transient amplitude in pig ventricular myocytes. In these animals, the duration of the Ca2+ transient was shortened probably secondary to the shorter action potential recorded in these myocytes [33]. Similar results were obtained in ventricular myocytes isolated from rats fed a diet rich in fish oil where Ca2+ transients and diastolic Ca2+ values remained unaltered in the presence of incorporated ω3-PUFAs. In this study, sarcoplasmic reticulum Ca2+ content was also unaffected by incorporated ω3-PUFAs [53].
In summary, the effects of acute administration of ω3-PUFAs on intracellular Ca2+ handling are different from those with incorporated ω3-PUFAs. Acute administration of ω3-PUFAs leads to a decrease in diastolic Ca2+ concentration in rat ventricular myocytes and in ventricular myocytes isolated from rabbits with heart failure [28,55,57]. Furthermore, EPA reduces spontaneous waves of Ca2+-release from the sarcoplasmic reticulum that underlie DAD-related arrhythmias [28,12]. Therefore, acute administration of ω3-PUFAs may reduce triggered activity based on spontaneous Ca2+-releases and DADs.
ω3-PUFAs have profound but various effects on cardiac electrophysiology, dependent on whether they circulate in the bloodstream (acute administration) or are incorporated into the sarcolemma of the myocyte (dietary intervention). Table 1 schematically summarizes ω3-PUFAs-induced changes in ion current densities and intracellular Ca2+ handling.
4. Pro- or antiarrhythmic effects in humans
Fish oil fatty acids EPA and DHA may be considered as electrophysiological drugs as they alter parameters important for the generation and maintenance of arrhythmias. Earlier antiarrhythmic drug trials were unsuccessful in reducing mortality in patients and in some cases, even increased mortality [14–17]. The negative outcomes in the antiarrhythmic drug trials were probably due to different mechanisms of arrhythmias of inhomogeneous patient populations. For example, the Cardiac Arrhythmia Suppression Trial (CAST) was designed to reduce ventricular ectopy in post myocardial infarction patients [16]. However, the initial effective suppression of ventricular ectopy by sodium channel blockers was followed by an increase in arrhythmic death in the following months [16]. Sodium channel blockade probably facilitates reentry by slowing conduction.
In line with the observations in CAST, ω3-PUFAs may also cause arrhythmias through sodium channels blockade and action potential shortening, two conditions that favour reentry-based arrhythmias [22]. Incorporated ω3-PUFAs shorten action potentials and thereby refractory periods [33] and acute administration of ω3-PUFAs slows ventricular conduction [34]. Therefore, arrhythmias based on reentry may occur more often in the presence of either circulating or incorporated ω3-PUFAs.
The conflicting outcomes of clinical trials with increased intake of fish oil regarding propensity to cardiac arrhythmias may be explained by inhomogeneous patient populations. The various patient subpopulations represent different arrhythmogenic mechanisms. Increased consumption of fish oil was antiarrhythmic in patients with a prior myocardial infarction. Likely, in this patient population, arrhythmias may have been based on triggered activity due to spontaneous Ca2+-releases and prolonged action potentials. Harmful effects of fish oil were seen in patients with acute ischemia and in patients with a history of sustained ventricular tachycardia/ventricular fibrillation. The arrhythmic mechanism in these patients may have been based on reentry.
5. Acute administration versus incorporation of ω3-PUFAs
Increased consumption of fish oil leads to increased (circulating) blood-levels of ω3-PUFAs [2] and ω3-PUFAs incorporation into various tissues [60]. The relative contributions of circulating and incorporated ω3-PUFAs to electrophysiology have not yet been discriminated.
Data on plasma levels of ω3-PUFAs after dietary interventions are scarce. In post menopausal women, fish oil supplements (2 g EPA and 1.4 g DHA) for 5 weeks increased plasma concentrations of EPA and DHA up to 0.5–0.7 mM [61]. In dogs, a fish oil rich diet for 8 weeks increased EPA and DHA serum levels to 1.0–1.3 mM [62]. To which extent these plasma levels are actually ‘free’ EPA and DHA, is unknown. Negretti et al. estimated that maximum levels of free circulating ω3-PUFAs are ∼8–32 μM [55].
Dietary administration of fish oil leads to the incorporation of ω3-PUFAs into all the membranes including myocardial membranes of the heart. Several weeks after the start of the dietary intervention with fish oil, ω3-PUFAs account for ∼25% of total lipids in the sarcolemma [33,53].
What are the primary sites of action of circulating and incorporated ω3-PUFAs? Leaf and coworkers showed that substitution of a single amino acid in the hH1α diminished the inhibitory effect of the acutely administered EPA on I Na [39], supporting a hypothesis of direct interaction between the fatty acid and ion channel. However, this explanation alone was unsatisfactory because other ligand gated ion channels that lack amino acid homology with voltage gated ion channels are also inhibited by an acute administration of ω3-PUFAs [63]. Therefore, it has been suggested that fatty acids primarily alter membrane properties close to ion channels rather than a direct interaction with the ion channel protein. Andersen and coworkers hypothesized that incorporation of the long acyl chain of the fatty acid compresses the phospholipid bilayer resulting in a mismatch with the hydrophobic length of the transmembrane channel [64]. The resulting compression or stretch by the long chain fatty acids will, therefore, alter the conformational state and conductance of the ion channel [65].
Another hypothesis is that acutely administered ω3-PUFAs alter membrane fluidity. Gating properties of I Na were altered by acute administration of ω3-PUFAs, but also by benzyl alcohol [40]. The latter compound is known to increase membrane fluidity [40]. In this study, block of I Na by ω3-PUFAs correlated with an increased membrane fluidity [40]. Nevertheless, another study debated the potency of PUFAs to alter membrane fluidity, since the molar ratio's of PUFAs to membrane phospholipids was found to be very low (<1%) [66].
Dietary administration of fish oil alters lipid rafts and specific microdomains of the plasma membrane [67]. There is an increasing body of evidence for significant ion channel localization in lipid rafts [68]. Incorporated ω3-PUFAs enhance the propensity to form PUFA-rich microdomains and would thereby modify the function of proteins [69].
Changes in intracellular pathways, alterations in cellular redox status, gene expression and metabolism of phosphoinositides have also been reported by ω3-PUFAs and are reviewed by Judé and coworkers [70].
6. Conclusions
1. Circulating ω3-PUFAs have different electrophysiological effects from ω3-PUFAs incorporated into the sarcolemma. 2. Fish oil ω3-PUFAs are cardiac electrophysiological drugs that may result in pro- or antiarrhythmia depending on the underlying arrhythmogenic mechanism. 3. An advice to increase intake of ω3-PUFA supplements or fatty fish should be tailored to individual patients regarding the arrhythmogenic mechanisms associated with their pathology.
Acknowledgements
The authors thank Professors M.J. Janse and M.B. Katan, Dr. A.C.G van Ginneken and Ed Hull for their valuable comments. This work was supported by the Netherlands Heart Foundation (2003B079) and SEAFOODplus program of the European Union (506359).
References
[1] Albert C.M. Hennekens C.H. O'Donnell C.J. Ajani U.A. Carey V.J. Willett W.C. Fish consumption and risk of sudden cardiac death JAMA 1998 279 23 28 [2] Albert C.M. Campos H. Stampfer M.J. Ridker P.M. Manson J.E. Willett W.C. Blood levels of long-chain n-3 fatty acids and the risk of sudden death N Engl J Med 2002 346 1113 1118 [3] Burr M.L. Gilbert J.F. Holliday R.M. Elwood P.C. Fehily A.M. Rogers S. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet And Reinfarction Trial (DART) The Lancet 1989 334 757 761 [4] GISSI-Prevenzione Investigators Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial The Lancet 1999 354 447 455 [5] Kris-Etherton P.M. Harris W.S. Appel L.J. for the Nutrition Committee Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease Circulation 2002 106 2747 2757 [6] Burr M.L. Ashfield-Watt P.A.L. Dunstan F.D.J. Lack of benefit of dietary advice to men with angina: results of a controlled trial Eur J Clin Nutr 2003 57 2 193 200 [7] Raitt M.H. Connor W.E. Morris C. Kron J. Halperin B. Chugh S.S. Fish oil supplementation and risk of ventricular tachycardia and ventricular fibrillation in patients with implantable defibrillators: a randomized controlled trial JAMA 2005 293 2884 2891 [8] Brouwer I.A. Zock P.L. Camm A.J. Bocker D. Hauer R.N.W. Wever E.F.D. Effect of fish oil on ventricular tachyarrhythmia and death in patients with implantable cardioverter defibrillators: the study on omega-3 fatty acids and ventricular arrhythmia (SOFA) randomized trial JAMA 2006 295 2613 2619 [9] Leaf A. Albert C.M. Josephson M. Steinhaus D. Kluger J. Kang J.X. Prevention of fatal arrhythmias in high-risk subjects by fish oil n-3 fatty acid intake Circulation 2005 112 2762 2768 [10] Hooper L. Thompson R.L. Harrison R.A. Summerbell C.D. Ness A.R. Moore H.J. Risks and benefits of omega 3 fats for mortality, cardiovascular disease, and cancer: systematic review BMJ 2006 332 752 760 [11] Janse M.J. Electrophysiological changes in heart failure and their relationship to arrhythmogenesis Cardiovasc Res 2004 61 208 217 [12] Baartscheer A. Schumacher C.A. Belterman C.N.W. Coronel R. Fiolet J.W.T. SR calcium handling and calcium after-transients in a rabbit model of heart failure Cardiovasc Res 2003 58 99 108 [13] Janse M.J. Wit A.L. Electrophysiological mechanisms of ventricular arrhythmias resulting from myocardial ischemia and infarction Physiol Rev 1989 69 1049 1169 [14] Boutitie F. Boissel J.P. Connolly S.J. Camm A.J. Cairns J.A. Julian D.G. Amiodarone interaction with β-blockers: analysis of the merged EMIAT (European Myocardial Infarct Amiodarone Trial) and CAMIAT (Canadian Amiodarone Myocardial Infarction Trial) databases Circulation 1999 99 2268 2275 [15] Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group Torp-Pederson C. Moller M. Bloch-Thomsen P.E. Kober L. Sandoe E. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group N Engl J Med 1999 341 857 865 [16] The Cardiac Arrhythmia Suppression Trial (CAST) Investigators Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction N Engl J Med 1989 321 406 412 [17] Waldo A.L. Camm A.J. deRuyter H. Friedman P.L. MacNeil D.J. Pauls J.F. Effect of d-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction The Lancet 1996 348 7 12 [18] Working Group on Arrhythmias of the European Society of Cardiology The Sicilian gambit. A new approach to the classification of antiarrhythmic drugs based on their actions on arrhythmogenic mechanisms. Task Force of the Working Group on Arrhythmias of the European Society of Cardiology Circulation 1991 84 1831 1851 [19] Hoffman B.F. Rosen M.R. Cellular mechanisms for cardiac arrhythmias Circ Res 1981 49 1 15 [20] Fozzard H.A. Afterdepolarizations and triggered activity Basic Res Cardiol 1992 87 105 113 [21] Nuss H.B. Kääb S. Kass D.A. Tomaselli G.F. Marban E. Cellular basis of ventricular arrhythmias and abnormal automaticity in heart failure Am J Physiol Heart Circ Physiol 1999 277 H80 H91 [22] Mines G.R. On circulating excitations in heart muscle and their possible relation to tachycardia and fibrillation Trans R Soc Can 1914 8 43 52 [23] McLennan P.L. Abeywardena M.Y. Charnock J.S. Dietary fish oil prevents ventricular fibrillation following coronary artery occlusion and reperfusion Am Heart J 1988 116 709 717 [24] McLennan P.L. Bridle T.M. Abeywardena M.Y. Charnock J.S. Dietary lipid modulation of ventricular fibrillation threshold in the marmoset monkey Am Heart J 1992 123 1555 1561 [25] Dujardin K. Dumotier B. Hondeghem L. Dietary supplementation with n-3 polyunsaturated fatty acids: a far less toxic alternative and perhaps superior antiarrhythmic therapy to amiodarone? (Abstract) Circulation 2005 112 U554 [26] Billman G.E. Kang J.X. Leaf A. Prevention of sudden cardiac death by dietary pure omega-3 polyunsaturated fatty acids in dogs Circulation 1999 99 2452 2457 [27] Schrepf R. Limmert T. Claus Weber P. Theisen K. Sellmayer A. Immediate effects of n-3 fatty acid infusion on the induction of sustained ventricular tachycardia The Lancet 2004 363 1441 1442 [28] Den Ruijter H.M. Berecki G. Belterman C.N.W. Schumacher C.A. Baartscheer A. Fiolet J.W.T. Fish oil reduces the number of calcium after-transients and delayed afterdepolarizations in isolated myocytes from rabbits with heart failure. (Abstract) Circulation 2005 112 1717 [29] Matthan N.R. Jordan H. Chung M. Lichtenstein A.H. Lathrop D.A. Lau J. A systematic review and meta-analysis of the impact of omega-3 fatty acids on selected arrhythmia outcomes in animal models Metabolism 2005 54 1557 1565 [30] Ander B.P. Weber A.R. Rampersad P.P. Gilchrist J.S.C. Pierce G.N. Lukas A. Dietary flaxseed protects against ventricular fibrillation induced by ischemia–reperfusion in normal and hypercholesterolemic rabbits J Nutr 2004 134 3250 3256 [31] Kang J.X. Free, long-chain, polyunsaturated fatty acids reduce membrane electrical excitability in neonatal rat cardiac myocytes Proc Natl Acad Sci 1995 92 3997 4001 [32] Macleod J.C. Macknight A.D.C. Rodrigo G.C. The electrical and mechanical response of adult guinea pig and rat ventricular myocytes to omega-3 polyunsaturated fatty acids Eur J Pharmacol 1998 356 261 270 [33] Verkerk A.O. van Ginneken A.C.G. Berecki G. Den Ruijter H.M. Schumacher C.A. Veldkamp M.W. Incorporated sarcolemmal fish oil fatty acids shorten pig ventricular action potentials Cardiovasc Res 2006 70 509 520 [34] Dhein S. Michaelis B. Mohr F.W. Antiarrhythmic and electrophysiological effects of long-chain omega-3 polyunsaturated fatty acids Naunyn-Schmiedeberg's Arch Pharmacol 2005 371 202 211 [35] Bogdanov K.Y. Spurgeon H.A. Vinogradova T.M. Lakatta E.G. Modulation of the transient outward current in adult rat ventricular myocytes by polyunsaturated fatty acids Am J Physiol Heart Circ Physiol 1998 274 H571 H579 [36] Cranefield P.F. The conduction of the cardiac impulse 1975 Mount Kisco, NY Futura Publishing Company Inc. [37] Xiao Y.F. Kang J.X. Morgan J.P. Leaf A. Blocking effects of polyunsaturated fatty acids on Na+ channels in neonatal rat ventricular myocytes Proc Natl Acad Sci 1995 92 11000 11004 [38] Xiao Y.F. Wright S.N. Wang G.K. Morgan J.P. Leaf A. Fatty acids suppress voltage-gated Na+ currents in HEK293t cells transfected with the alpha subunit of the human cardiac sodium channel Proc Natl Acad Sci 1998 95 2680 2685 [39] Xiao Y.F. Ke Q. Wang S.Y. Auktor K. Yang Y. Wang G.K. Single point mutations affect fatty acid block of human myocardial sodium channel alpha subunit Na+ channels Proc Natl Acad Sci 2001 98 3606 3611 [40] Leifert W.R. McMurchie E.J. Saint D.A. Inhibition of cardiac sodium currents in adult rat myocytes by n-3 polyunsaturated fatty acids J Physiol 1999 520 671 679 [41] Xiao Y.F. Ma L. Wang S.Y. Josephson M. Wang G.K. Morgan J.P. Potent block of inactivation-deficient Na+ channels by n-3 polyunsaturated fatty acids Am J Physiol Cell Physiol 2006 290 C362 C370 [42] Leifert W.R. Jahangiri A. Saint D.A. McMurchie E.J. Effects of dietary n-3 fatty acids on contractility, Na+ and K+ currents in a rat cardiomyocyte model of arrhythmia J Nutr Biochem 2000 11 382 392 [43] Xiao Y.F. Gomez A.M. Morgan J.P. Lederer W.J. Leaf A. Suppression of voltage-gated L-type Ca2+ currents by polyunsaturated fatty acids in adult and neonatal rat ventricular myocytes Proc Natl Acad Sci 1997 94 4182 4187 [44] Ferrier G.R. Redondo I. Zhu J. Murphy M.G. Differential effects of docosahexaenoic acid on contractions and L-type Ca2+ current in adult cardiac myocytes Cardiovasc Res 2002 54 601 610 [45] Danthi S.J. Enyeart J.A. Enyeart J.J. Modulation of native T-type calcium channels by omega-3 fatty acids Biochem Biophys Res Commun 2005 327 485 493 [46] Antzelevitch C. Sicouri S. Litovsky S.H. Lukas A. Krishnan S.C. Di Diego J.M. Heterogeneity within the ventricular wall. Electrophysiology and pharmacology of epicardial, endocardial, and M cells Circ Res 1991 69 1427 1449 [47] Singleton C.B. Valenzuela S.M. Walker B.D. Tie H. Wyse K.R. Bursill J.A. Blockade by n-3 polyunsaturated fatty acid of the Kv4.3 current stably expressed in Chinese hamster ovary cells Br J Pharmacol 1999 127 941 948 [48] Xiao Y.F. Morgan J.P. Leaf A. Effects of polyunsaturated fatty acids on cardiac voltage-activated K+ currents in adult ferret cardiomyocytes Sheng Li Xue Bao 2002 54 271 281 [49] Judé S. Bedut S. Roger S. Pinault M. Champeroux P. White E. Peroxidation of docosahexaenoic acid is responsible for its effects on ITO and ISS in rat ventricular myocytes Br J Pharmacol 2003 139 816 822 [50] Guizy M. Arias C. David M. Gonzalez T. Valenzuela C. Omega-3 and omega-6 polyunsaturated fatty acids block HERG channels Am J Physiol Cell Physiol 2005 289 C1251 C1260 [51] Doolan G.K. Panchal R.G. Fonnes E.L. Clarke A.L. Williams D.A. Petrou S. Fatty acid augmentation of the cardiac slowly activating delayed rectifier current (I Ks ) is conferred by hminK FASEB J 2002 12 1662 1664 [52] Xiao Y.F. Ke Q. Chen Y. Morgan J.P. Leaf A. Inhibitory effect of n-3 fish oil fatty acids on cardiac Na+/Ca2+ exchange currents in HEK293t cells Biochem Biophys Res Commun 2004 321 116 123 [53] Leifert W.R. Dorian C.L. Jahangiri A. McMurchie E.J. Dietary fish oil prevents asynchronous contractility and alters Ca2+ handling in adult rat cardiomyocytes J Nutr Biochem 2001 12 365 376 [54] Pogwizd S.M. Bers D.M. Cellular basis of triggered arrhythmias in heart failure Trends Cardiovasc Med 2004 14 61 66 [55] Negretti N. Perez M.R. Walker D. O'Neill S.C. Inhibition of sarcoplasmic reticulum function by polyunsaturated fatty acids in intact, isolated myocytes from rat ventricular muscle J Physiol 2000 523 367 375 [56] Swan J.S. Dibb K. Negretti N. O'Neill S.C. Sitsapesan R. Effects of eicosapentaenoic acid on cardiac SR Ca2+-release and ryanodine receptor function Cardiovasc Res 2003 60 337 346 [57] O'Neill S.C. Perez M.R. Hammond K.E. Sheader E.A. Negretti N. Direct and indirect modulation of rat cardiac sarcoplasmic reticulum function by n-3 polyunsaturated fatty acids J Physiol 2002 538 179 184 [58] Honen B.N. Suppression of calcium sparks in rat ventricular myocytes and direct inhibition of sheep cardiac RyR channels by EPA, DHA and oleic acid J Membr Biol 2003 196 95 103 [59] Verkerk A.O. Veldkamp M.W. Baartscheer A. Schumacher C.A. Klopping C. van Ginneken A.C.G. Ionic mechanism of delayed afterdepolarizations in ventricular cells isolated from human end-stage failing hearts Circulation 2001 104 2728 2733 [60] Kitajka K. Sinclair A.J. Weisinger R.S. Weisinger H.S. Mathai M. Jayasooriya A.P. Effects of dietary omega-3 polyunsaturated fatty acids on brain gene expression Proc Natl Acad Sci 2004 101 10931 10936 [61] Higdon J.V. Liu J. Du S.H. Morrow J.D. Ames B.N. Wander R.C. Supplementation of postmenopausal women with fish oil rich in eicosapentaenoic acid and docosahexaenoic acid is not associated with greater in vivo lipid peroxidation compared with oils rich in oleate and linoleate as assessed by plasma malondialdehyde and F(2)-isoprostanes Am J Clin Nutr 2000 72 714 722 [62] Hansen R.A. Ogilvie G.K. Davenport D.J. Gross K.L. Walton J.A. Richardson K.L. Duration of effects of dietary fish oil supplementation on serum eicosapentaenoic acid and docosahexaenoic acid concentrations in dogs Am J Vet Res 1998 59 864 868 [63] Leaf A. Xiao Y.F. Kang J.X. Interactions of n-3 fatty acids with ion channels in excitable tissues Prostaglandins Leukot Essent Fatty Acids 2002 67 113 120 [64] Girshman J. Greathouse D.V. Koeppe R.E. Andersen O.S. Gramicidin channels in phospholipid bilayers with unsaturated acyl chains Biophys J. 1997 73 1310 1319 [65] Lundbaek J.A. Andersen O.S. Spring constants for channel-induced lipid bilayer deformations. Estimates using gramicidin channels Biophys J 1999 76 889 895 [66] Pound E.M. Kang J.X. Leaf A. Partitioning of polyunsaturated fatty acids, which prevent cardiac arrhythmias, into phospholipid cell membranes J Lipid Res 2001 42 346 351 [67] Fan Y.Y. McMurray D.N. Ly L.H. Chapkin R.S. Dietary (n-3) polyunsaturated fatty acids remodel mouse T-cell lipid rafts J Nutr 2003 133 1913 1920 [68] Maguy A. Hebert T.E. Nattel S. Involvement of lipid rafts and caveolae in cardiac ion channel function Cardiovasc Res 2006 69 798 807 [69] Ma D.W.L. Seo J. Switzer K.C. Fan Y.Y. McMurray D.N. Lupton J.R. n-3 PUFA and membrane microdomains: a new frontier in bioactive lipid research J Nutr Biochem 2004 15 700 706 [70] Judé S. Roger S. Martel E. Besson P. Richard S. Bougnoux P. Dietary long-chain omega-3 fatty acids of marine origin: a comparison of their protective effects on coronary heart disease and breast cancers Prog Biophys Mol Biol 2006 90 299 325
Author notes
Copyright © 2006, European Society of Cardiology